Newly published research associating poor quality sleep with a greater risk of glaucoma offers further evidence that eye health – and, more specifically, health of the retina — is linked to the body’s most basic and important physiologic processes, says an internationally renowned optometric scientist, specializing in retinal processing at the Mind-Eye Institute in Northbrook, Illinois.
“The retina is composed of brain tissue and functions as part of the body’s central nervous system. For this reason, all body processes connect with the eye in some way, including the endocrine, neurological, psychiatric, respiratory, musculoskeletal, and gastrointestinal systems; and, of course, sleep,” explains Deborah Zelinsky OD. Dr. Zelinsky is founder and executive director of research for the Mind-Eye Institute.
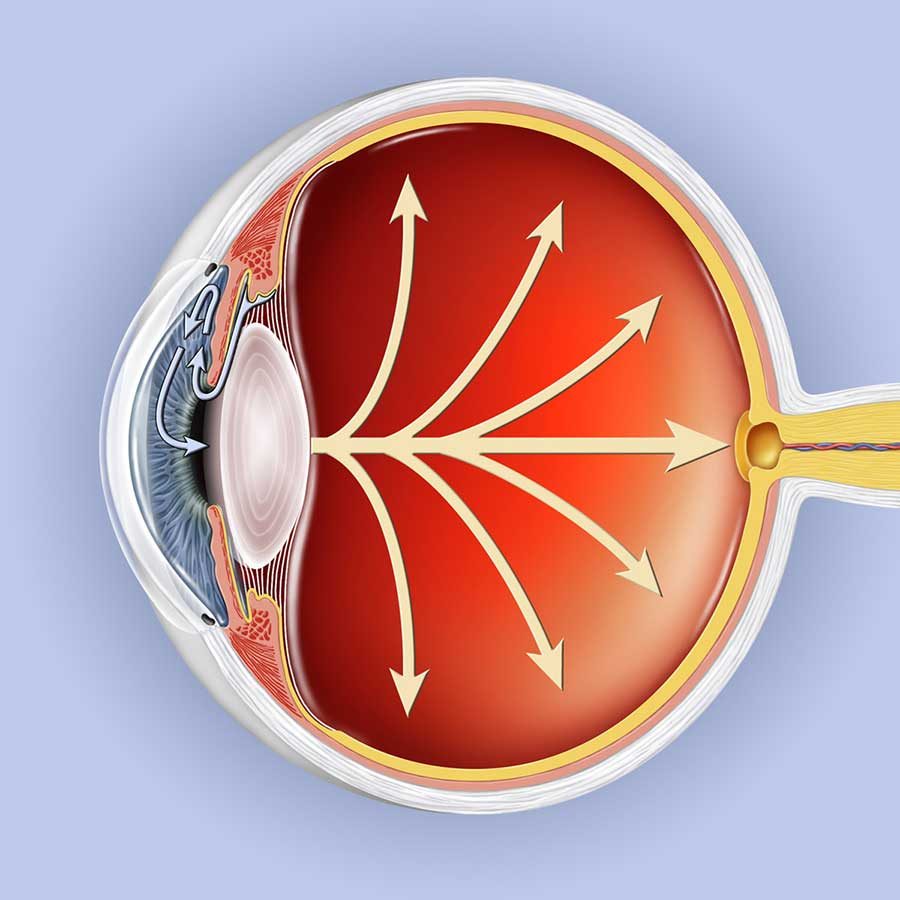
“Light is the way in which the retina communicates with the brain. The light triggers electrical signals that propagate through nerves affecting critical brain structures.” Glaucoma is a major cause of blindness in the United States. The disease is related to
increased intraocular pressure. That pressure can damage some of the optic nerve’s neurons through which light-sensor signals from the retina are funneled.
In a study, published online in a 2022 fall issue of the journal BMJ, scientists conclude “individuals with suboptimal sleep patterns…, characterized by snoring and daytime sleepiness or insomnia and short/long sleep duration, [are] at increased risk of glaucoma.” The investigative team proposed that altered hormonal balances and mood disorders like anxiety and depression — all associated with insomnia and other sleep disorders — play a role in elevating intraocular pressure (IOP). Heightened IOP increases risk of developing glaucoma. “Further, insomnia and its related stress response may stimulate neurotransmitter secretion and the autonomic nervous system, influencing the regulation of IOP and blood flow. Decreased ocular blood flow is a well-known risk factor for the development and progression of glaucoma,” study authors write. Their research involved recruitment of more than 400,000 study participants over multiple years.
The latest findings are not surprising, says Dr. Zelinsky, who refers to a survey of nearly 6,800 patients with glaucoma and corresponding visual field defects. From the patients’ responses, reported in 2019, scientists determined an association exists between glaucoma and poor sleep architecture, including sleep of abnormal duration and latency and excessive daytime sleepiness. Another investigation, published in 2020 in the Journal of Glaucoma, suggests “impaired perception of light input due to glaucoma can subsequently lead to abnormal serum levels of melatonin, [a hormone released at night by the brain’s pineal gland and also directly within the retina], resulting in circadian rhythm misalignment. This disruption of the circadian rhythm also contributes to sleep and mood disorders [that are] common in individuals with glaucoma.”
The retina not only transmits environmental signals for eyesight at a conscious level, but also from external light levels and movement detected by the retina at a subconscious level,” Dr. Zelinsky relates. “Concurrently, the retina receives feedback signals from the body. This continual process of feeding forward sensory signals to the brain from the environment and then receiving feedback signals from various brain structures makes the retina a two-way portal for influencing and monitoring thought processes, internal organs, and basic functions, such as posture, movement, and motor reflexes.”
Any disruption of the retina’s functions can negatively impact the integration of a person’s sensory systems, including eye-ear connections, and visual processing capabilities. Visual processing relates to that almost instantaneous ability of the brain to take in multiple sensory signals (from eyesight, hearing, smell, taste, and touch) at all levels – unconscious, subconscious, and conscious; meld them with an individual’s internal sensory signals; and then process the information to create a response.
The Mind-Eye Institute is noted worldwide for its use of individualized, therapeutic brain glasses, and other optometric interventions to help patients redevelop visual processing skills during recovery from brain injuries and neurological disorders, including concussion and strokes, or to build new processing skills in patients labeled as having “learning differences.” Mind-Eye brain glasses work by bending and changing how light passes through the retina. The glasses vary the intensity, angle, and amount of light in an effort to bring relief to patients suffering from a variety of symptoms such as light sensitivity, attention and concentration deficits, and poor depth perception, Dr. Zelinsky says.
“Glaucoma is a serious disorder that is now being considered as a neurodegenerative disease process – in the same category as Parkinson’s and Alzheimer’s diseases. This latest 2022 study helps increase our understanding of the disease and opens the door to potential new ways for treating and preventing it in the future,” Dr. Zelinsky concludes.
image from Glaucoma Research Foundation