Key Takeaways
- Dizziness is a common post-concussion symptom and may indicate delayed neurological recovery.
- Symptoms can stem from multiple systems—vestibular, visual, proprioceptive, cervical, and autonomic.
- Disrupted sensory integration, especially between the eyes and ears, often leads to vertigo and balance issues.
- The vestibulo-ocular reflex (VOR) is critical for stabilizing vision and posture; injury can worsen dizziness.
- The Mind-Eye Institute uses specialized lenses and tools like the Z-Bell Test™ to help restore sensory harmony and reduce symptoms.
- 90% of compliant Mind-Eye patients improved dizziness since 2022
Dizziness is second only to headaches as a symptom following concussion or traumatic brain injury. According to an article in Frontiers in Neurology, dizziness can be “predictive of a prolonged recovery from post-concussive syndrome.” But what constitutes dizziness? Experts call the symptom “ill-defined.” Patients describe the sensation in diverse ways, sometimes associating it with “giddiness;” feeling light-headed, “woozy,” or faint; unsteadiness; being off-balance; or a sense that one is spinning or the world is spinning (vertigo).
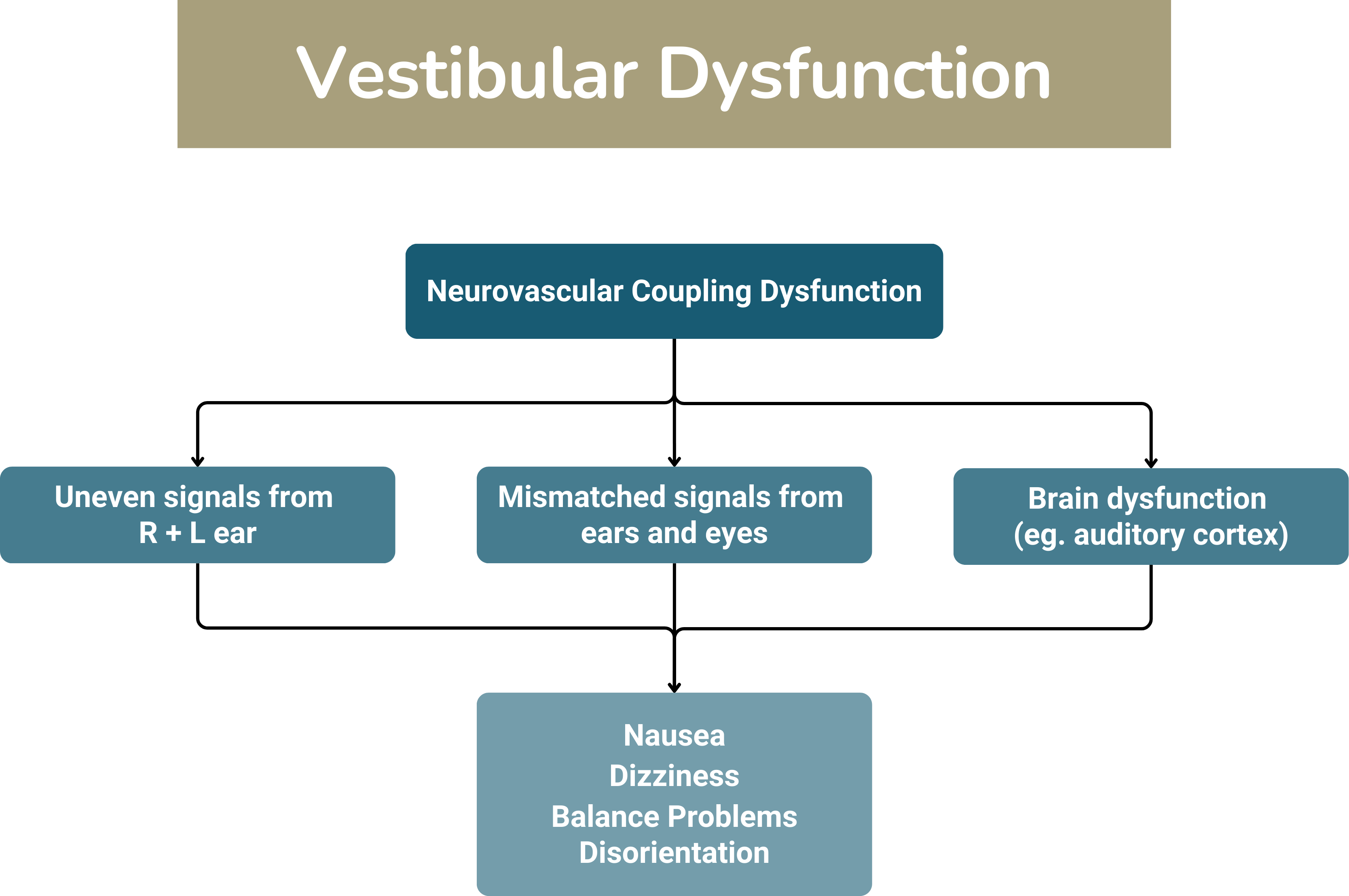
Variations in description occur because dizziness can develop as a result of multiple issues depending on what was affected by a person’s closed head injury. A blow to the head interferes with brain function – at least temporarily – disrupting the brain’s nerve signals. The severity of the injury and its location can determine what is affected. In the words of some health professionals, dizziness is caused by disruption in “how the brain processes input from and output to your eyes, ears, and body; concurrent injury to your neck, inner ear, or visual system; post-traumatic migraines (another common symptom after concussion); spatial disorientation; or decreased tolerance to physical activity [namely, exercise].”
Deborah Zelinsky OD, founder and executive research director of the Mind-Eye Institute, in the Chicago suburb of Northbrook, says head injury and disease may disrupt integration and coordination of a person’s senses, especially eyes and ears. When the work of eyes and ears is no longer synchronized, then the result oftentimes is abnormal visual processing and development of symptoms such as headaches, dizziness, and vertigo. “If the brain fails to function efficiently, busy environments – sights, sounds, smells, and movement, [including the movement of other people] -- can literally cause one to become dizzy, nauseous, confused, stressed.”
Types of Dizziness Following Concussion or Traumatic Brain Injury
- Peripheral Vestibular Injury: Should a concussion disturb the inner ear or the vestibular nerve – the nerve responsible for carrying balance signals to the brain, a patient will experience dizziness and vertigo that make if difficult to walk in a steady manner or stand or sit upright. The injury also may cause tinnitus (ringing in the ears), hearing loss, and eye movements.
- Central Vestibular Injury: Head trauma damages structures in the brain that participate in the vestibular system and are responsible for maintaining balance.
- Visual System Disruption: A concussion can damage the visual system’s ability to “track where the body is in space and in what direction it is moving.” During movement, the “brain reassesses [a person’s] relationship” to near and far objects in the area. Disruption of the visual system can lead to vertigo and dizziness.
- Cervical Vertigo: If a head injury also affects the neck muscles and vertebrae, a person may develop resulting dizziness until the neck trauma resolves.
- Lack of Synchronicity between vestibular and visual systems: A concussion can cause what experts call a “mismatch” between vestibular (hearing) and visual (eyesight) systems. The mismatch means the “brain is getting conflicting information…: the information coming from the eyes does not match the information coming from the ears. Without reliable information, the brain has a hard time figuring out which is moving — you or the things around you."
- Injury to the Autonomic Nervous System: The autonomic nervous system regulates key internal organs and processes, including heart, kidneys, breathing rate, body temperature, digestion, and metabolism. If a head injury causes this system to become dysfunctional – dysautonomia, dizziness, vertigo, and balance problems can develop.
- Proprioceptive System Impairment: Scientists at the Cleveland Clinic describe the proprioceptive system as the “body’s ability to sense its own position and movements. It is an automatic or subconscious process. Proprioception allows the brain to know the position of your body in space without having to rely on visual input alone. It is also crucial to maintaining balance” Impairment of this system due to a concussion or traumatic brain injury can result in vertigo, dizziness, and imbalance.
- Dysfunction of the Vestibulo-Ocular Reflex: The vestibulo-ocular reflex (VOR) plays a significant role in balance, providing an important feedback pathway between eyes and inner ears. The VOR helps further prevent falls by providing head and postural stability because of the ongoing interaction among tactile, auditory, and proprioceptive sensory inputs. When injured, a patient will experience episodes of dizziness and balance problems.
Why Head Injury Can Affect Integration of Systems and Prove So Dizzying!
“Vestibular information is integrated with proprioceptive and other sensory inputs to generate our sense of motion,” say authors of a recent study, published in a 2021 issue of Current Opinion in Physiology. That is why patients with vestibular sensory loss or other vestibular impairments find “everyday activities like walking” to be difficult. “Even small head movements can produce postural and perceptual instability,” they state. In fact, among scientists and health professionals, a new term for this type of problem is – “Triple P” -- Persistent Postural-Perceptual Dizziness.
“Even small head movements can produce postural and perceptual instability."
— From Current Opinion in Physiology on persistent dizziness
The scientists’ description of how the proprioceptive and vestibular systems “work together” to help us navigate and move through our environment is not surprising. In fact, the author of a 2022 online article defines the vestibular system as a “somatosensory portion of the nervous system,” providing us “with the awareness of the spatial position of our head and body (proprioception) and self-motion (kinesthesia).”
Eye movements are linked at a reflex level to head movements! When head injury occurs or neurological disorders like Parkinson’s and Alzheimer’s disease develop, communication between neuron signals is often disrupted. And this disruption may then disturb the integration of these neurons with other body proprioceptors involving touch, sensation, pressure, and movement.
Experts often call proprioception an “internal sense.” Proprioceptors are mechanosensory neurons found within muscles, ligaments, tendons, and joints. They transmit information to the central nervous system and, in turn, activate feedback loops. These feedback loops allow the body to move without conscious attention. At the same time, they communicate with proprioceptor-like neurons in other sensory systems, including the ears and eyes. The integrated function and coordination of these neurons are what stabilize posture and prompt body movement. The proprioceptors help with balance, stair climbing, and core posture control, thereby lessening clumsiness.
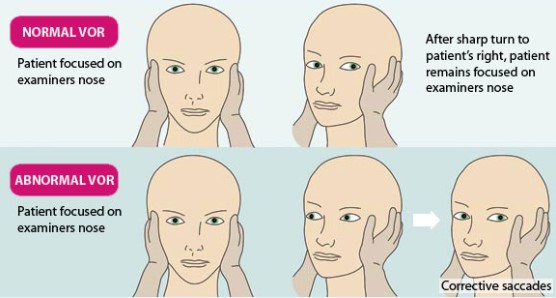
Figure from 360neurohealth.com
Although the vestibulo-ocular reflex is not specifically a part of the proprioceptive system, scientists writing in a recently published book Neuroanatomy, Vestibulo-ocular Reflex state “this reflex keeps us steady and balanced even though our eyes and head are continuously moving when we perform most actions.” When moving the head, “eye muscles are triggered instantly to create an eye movement opposite to that of our head movement at the exact same speed to readjust the visual world.” That adjustment, “in turn, stabilizes our retinal image by keeping the eye still in space and focused on an object, despite the head motion.”
Head injury can destabilize posture and balance by affecting this interactive VOR pathway. In the Encyclopedia of Behavioral Neuroscience (2010), authors write the “VOR uses information from the vestibular labyrinth of the inner ear to generate eye movements that stabilize gaze during head movements. Without the VOR, when walking down the street, it [would be] impossible [for a person] to read signs or even recognize faces.” VOR disturbances resulting from disease or brain injury can cause vertigo, spatial disorientation, and balance issues. Persons also may experience temporary impairment of proprioceptive neurons because of exhaustion, mental disorders like depression, vitamin and hormonal deficiencies, and cytotoxic factors, such as chemotherapy.
Head injury can destabilize posture and balance by affecting this interactive VOR pathway. In the Encyclopedia of Behavioral Neuroscience (2010), authors write the “VOR uses information from the vestibular labyrinth of the inner ear to generate eye movements that stabilize gaze during head movements. Without the VOR, when walking down the street, it [would be] impossible [for a person] to read signs or even recognize faces.” VOR disturbances resulting from disease or brain injury can cause vertigo, spatial disorientation, and balance issues. Persons also may experience temporary impairment of proprioceptive neurons because of exhaustion, mental disorders like depression, vitamin and hormonal deficiencies, and cytotoxic factors, such as chemotherapy.
Diagnosis of Dizziness and Imbalance
The Mind-Eye Institute has been studying the retina’s critical role in integrating various sensory maps, including eye-ear coordination, to process visual space and achieve proper spatial awareness. Synchronization of perceived auditory and visual space with proprioceptors optimizes performance. For instance, people can be scared of walking on stairs or through doorways. Another example is picking up objects, an action requiring subconscious planning of the amount of energy to exert. If the eyes send signals indicating something is going to be heavy, a person readies his or her arms to lift in a manner much different than when anticipating picking up a small box of feathers.
Visual processing involves a complex network of communication signals between the central nervous system (which includes the retina, brain, and spinal cord) and other circuitry, such as the emotional, motor, and sensory systems and thinking processes. Development of dizziness or vertigo is a symptom of disrupted visual processing and out-of-sync sensory systems, including oculomotor (eye movement) abnormalities.
Health professionals indicate dizziness and vertigo symptoms following a concussion or mild TBI usually resolve on their own within several weeks of the injury. Patients can facilitate their own recovery by keeping a regular sleep schedule, limiting computer and phone screen time, and resting in a darkened room. However, if symptoms persist, patients are advised to contact their physician. Diagnosis of the source of dizziness may require:
Eye movement tests.
“Balance tests that measure what happens when you get less input from your visual or proprioceptive systems; for example, by asking you to stand on a soft surface or a moving platform with your eyes closed.”
Computed tomography and magnetic resonance imaging of the head.
Blood tests.
Management of Dizziness
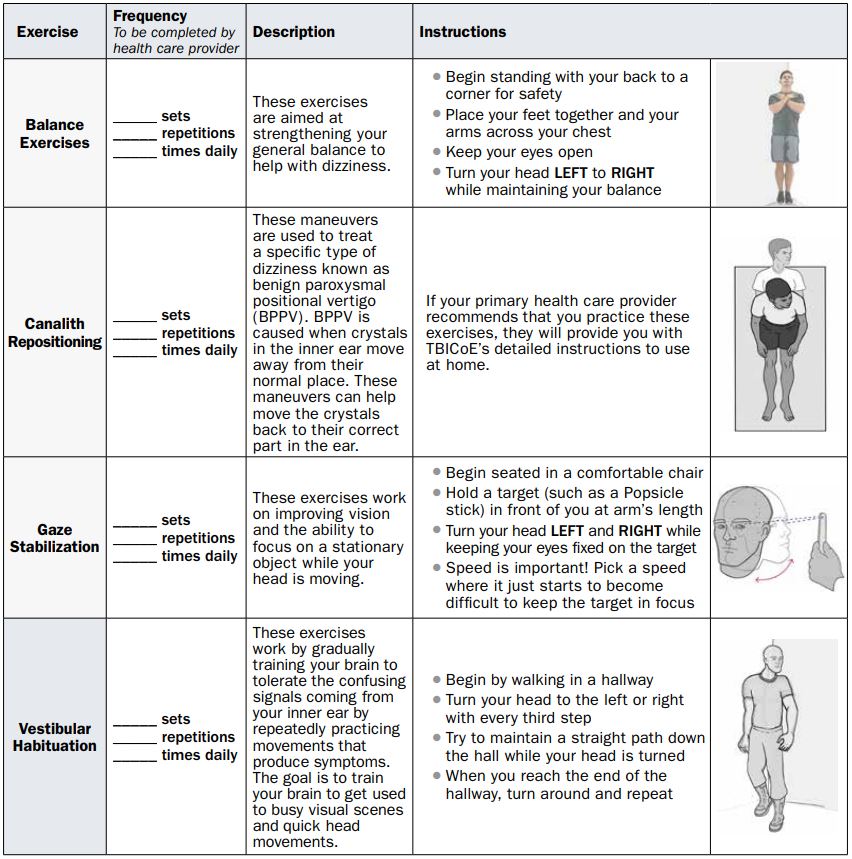
From the Managing Dizziness Following Concussion/Mild Traumatic Brain Injury Fact Sheet provided by the Military Health System.
Treatments for dizziness and vertigo vary depending on the diagnosed source of the problem. A doctor may recommend certain medications or general rest or may suggest one of the following protocols:
Eye and head movement exercises.
Vestibular rehabilitation therapy, which includes eye movement control, balance and gait training, and stretching and strengthening exercises.
Neuromuscular therapies to correct muscle dysfunctions, particularly that of the neck if it was also affected by a concussion.
Canalith repositioning to correct inner-ear issues by changing – or removing – crystals in the inner ear.
Even more unique and advanced approaches have been developed – and continue to be refined – to mitigate post-concussion syndrome, including dizziness. Specifically, the clinical work of the Mind-Eye Institute and the team’s use of therapeutic eyeglasses, lenses, prisms, filters, and other optometric tools has drawn global attention and attracted patients from throughout the world.
About the Mind-Eye Institute
Because the retina plays such a key role in the central nervous system, altering the way light enters the retina through the use of specialized lenses can:
Create changes in brain activity by often mitigating symptoms from traumatic head injury, concussion, stroke, or neurological disorders. These symptoms include visual processing disorders, headaches, brain fog, concentration and attention problems, sleep difficulties, even balance and mobility challenges.
Oftentimes prove effective in building undeveloped visual processing skills in children – and adults – with autism spectrum disorder, attention deficit hyperactivity disorder, and other learning difficulties.
Modify some internal systems that regulate metabolism, motor control, posture, mood, circadian rhythm, and decision-making abilities, among other processes.
A person’s sensory systems are like musicians in an orchestra. Each musician may be highly skilled in a specific instrument, but without a conductor synchronizing what they are playing, the result is simply noise – not music.
Brain injury and neurological disorders like Alzheimer’s disease disrupt sensory circuitry and mapping of space. When either central or peripheral eyesight fail to interact appropriately and/or inputs from eyes and ears are out of synchronization, patients often become confused about their environment. This confusion can create a narrowed perception and awareness of surroundings, inappropriate reactions and responses, and difficulties with decision-making skills, as well as learning and memory.
The Mind-Eye Institute’s internationally recognized and patented Z-Bell Test™ was developed and designed to evaluate a patient’s overall integration of retinal processing with awareness of auditory space – basically, the stability of the eye-ear connection. During the auditory portion of the test, a patient reaches out, with eyes closed, and tries touching a ringing bell. If the patient cannot do so, a Mind-Eye optometrist determines the optimal combination of lenses to place in front of the patient’s closed eyelids allowing the patient to find the bell immediately without conscious effort. Light still passes through the eyelids and activates parts of the brain not used for eyesight. With eyes closed, patients must visualize surrounding space in order to locate the bell. The optometrist repeats this with the visual portion of the testing.
Auditory localization and visual localization must match in order to lessen overall effort and sensory confusion and achieve normal proprioception. Brain-injured stroke patients, for example, often struggle with gaze stability. Hampered vestibulo-ocular reflex (VOR) function reduces dynamic visual acuity and causes balance issues. Imagine having to stare at your feet in an effort to maintain balance; you would not be able to process surrounding space easily or navigate and plan movements.
Real Patient Application
"I could not concentrate on conversations; I had a hard time focusing on what someone would be saying to me. If a ticker tape of information started crossing the bottom of the screen while I was watching television, I would become overwhelmingly dizzy. And watching movies on a large screen – that was devastating. Too much information. Mind-boggling.”
Relevant Research
Page [tcb_pagination_current_page] of [tcb_pagination_total_pages]
Interested in learning more?
At the Mind-Eye Institute we understand that interactions between the electrical and biochemical pathways in the brain affect physical, physiological and psychological systems. Visual interventions that alter retinal signaling pathways impact both the electrical and biochemical systems.
To learn about next steps for registering as a patient or registering a child as a patient, please call the Mind-Eye Institute office at 847.558.7817 or you can fill out our online New Patient Inquiry Form provided here.