Seeing the Brain Through the Eye is the title of a project underway in the laboratory of Delia Cabrera DeBuc PhD. at the prestigious Bascom Palmer Eye Institute of the University of Miami.
I refer to this scientific initiative because, first, its title effectively describes the latest, revolutionary phase of eye care and signifies why health care’s future path may soon begin with – and pass through — the eye care field.
Secondly, Dr. Cabrera DeBuc is among specialists on the cusp of creating a groundbreaking understanding of the role of the retina in health. She is leading development of tools needed to “enhance ocular imaging and imaging processing analysis” and “identify novel imaging biomarkers of the onset and progression of ophthalmic and neurological diseases using advanced optical imaging,” as reported in a narrative on the Bascom Palmer Eye Institute website.
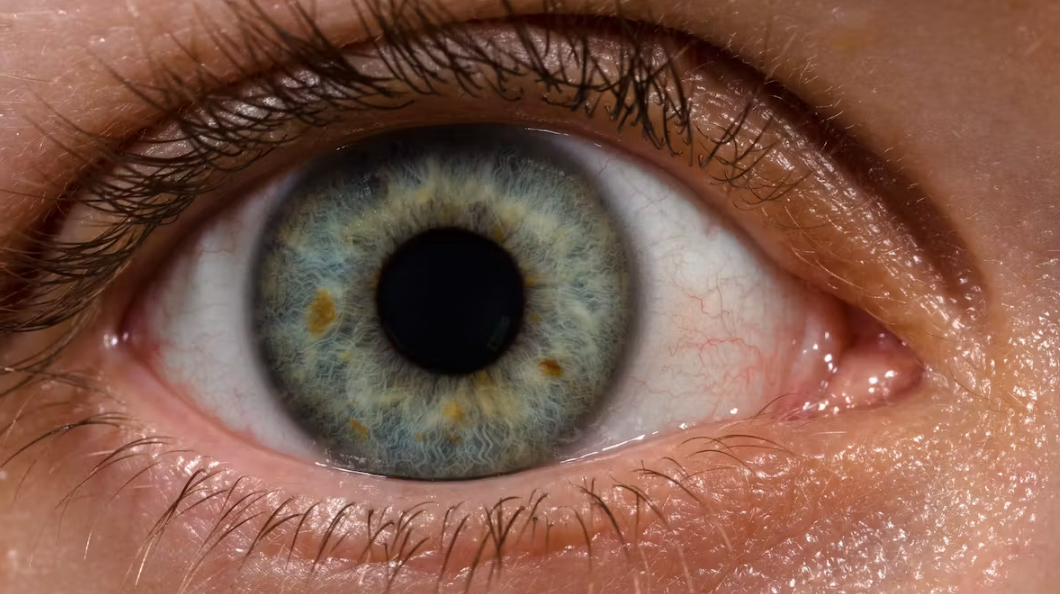
Scientists are quickly uncovering the secrets of the retina and using those secrets to open wider the window to the brain. That “window” is giving optometrists, physicians, and other health professionals the capability of evaluating a patient’s overall health through the eye and finding indications of multiple diseases for earlier treatment.
Sounds heavy? Well, it is. In fact, as the newly elected president of the Society for Brain Mapping & Therapeutics (SBMT), I am becoming increasingly involved in oculomics, the study of ophthalmic biomarkers and their association with various disorders. I have the privilege of co-chairing SBMT’s visual processing subcommittee with Dr. Cabrera DeBuc.
We already know that, through the eye, we can evaluate the body’s microvascular and neurosensory systems, finding evidence of hypertension, diabetes, colon cancer, and even presence of neurological disorders like Alzheimer’s and Parkinson’s disease. For example, one recent study of 46,000 people used images of the retina to accurately predict retinal age. The findings, published in a 2021 issue of the British Journal of Ophthalmology, show that the gap between a person’s retinal age and chronological age may be a “potential biomarker of aging that is closely related to mortality,” study authors state. “Each one-year increase in the retinal age gap was associated with a 2 percent increase in all-cause mortality…”
Diagnostic opportunities also continue expanding with the advent of recent technological innovations and breakthroughs, such as artificial intelligence and the Kernel Flow.
In a 2022 issue of the journal Frontiers, authors call the eye a “uniquely accessible window that allows direct visualization of neuro-vasculature using noninvasive imaging modalities.” They indicate artificial intelligence (AI) analytics — as applied to images of a person’s eye – can help predict “demographic parameters, body composition factors, and diseases of the heart, blood, nerves, energy, hormones, kidney and liver systems…Many neurodegenerative conditions that involve the brain and spinal cord have ocular manifestations.” Although “ophthalmic AI models for predicting systemic disease [compose] a novel field in its nascency…there is great capacity for translation into wider practice in the future,” the scientists write.
Among the latest technological advancements is the Kernel Flow, a monitoring device for brain activity. It is designed as a wearable headset developed by the neurotechnology company, Kernel. The technology uses noninvasive, time-domain near-infrared spectroscopy (TD-fNIRS) to measure changes in the oxygenation of blood in the brain.
“TD-fNIRS has been considered the gold standard of noninvasive optical brain imaging devices. However, [until now], due to high cost, complexity, and large form factor, it has not been widely adopted as continuous-wave NIRS systems,” according to authors of a 2022 article in the Journal of Biomedical Optics. “The miniaturized design of the Kernel Flow system [now] allows for broader applications of TD-fNIRS.”
As the 2023 leader of SBMT, my mission is to make optometry a go-to field for neurological and biochemical research. This can be achieved by bringing new technologies to the forefront – like the Kernel Flow – which can significantly expand optometrists’ health care abilities and by promoting a greater understanding of how optometrists might use individualized eyeglasses and other pioneering optometric approaches to impact brain activity. Achieving these goals will increase awareness of optometry’s potential impact on brain function and change current standards of patient care in optometry.
Peripheral eyesight is highly utilized in our modernized society of busy traffic, flashing signs, crowded stores, moving displays, and scrolling GPS and computer screens. Most of my 35-plus-year career in optometry has been devoted to developing – and applying — advanced optometric methods for assessing peripheral eyesight and brain function, with emphasis on the often-untested linkage between eyes and ears. The addition of many new peripheral eyesight assessments to existing 20/20 central eyesight testing will help many patients who have brain injuries and/or autonomic dysfunctions. For such patients, 20/20 testing alone is not enough to achieve a comfortable eyeglass prescription. Frequently, people who have 20/20 without any eyeglasses still require lenses for efficient brain activity and visual processing.
When intact, visual processing enables people to understand and interact appropriately with the world around them. If brain circuitry is out of sync because it has been disrupted by trauma or disease or is underdeveloped, people can become confused about their surrounding environment and exhibit inappropriate reactions and responses. If eyes and ears are not integrated, people have to continuously shift attention, and that effort becomes exhausting.
Eye-ear integration is the concept underlying our clinical work and experience at the Mind-Eye Institute. Our team uses therapeutic lenses, filters, and other optometric interventions to change the way light passes through the retina (which is made of brain tissue and part of the central nervous system), thereby affecting how the brain reacts to information about the environment. Modifying the way in which light strikes the retina oftentimes brings relief and helps patients suffering symptoms of brain injury, stroke, and other neurological diseases or struggling with learning disorders due to underdeveloped visual processing skills.
Since World War II, optometry has gone through several important shifts. After the war ended, optometrists served as ocular technicians, sharpening eyesight to 20/20 by fitting patients with glasses. Twenty years later, four years of specialized education were required to practice optometry. By the 1980s, optometrists were dilating eyes in order to better examine them. Today’s 21st century optometrists now have access to advanced tools and research, giving them the power to help shape the future of health care in general.
The Mind-Eye Institute is at the cutting edge of the “new optometry.” We are not just simply doing eye care anymore, but working with neuroscientists, ophthalmologists, endocrinologists, internists, psychiatrists, biochemists, and ocular researchers to enhance ophthalmic approaches to improved diagnosis, treatment, and prevention of disease. Concurrently, we are working with ancillary professions, such as physical therapy, occupational therapy, Neuromovement® reflex integration therapy, and integrative manual therapy, among others.
Know that Dr. Delia Cabrera DeBuc’s “Seeing the Brain Through the Eye” is more than a slogan or a project title. It describes the 21st century of optometry. Now is the time to “Leave 20/20 in the 20th century” — an achievable goal, thanks to Dr. Cabrera DeBuc’s brilliant work and the Mind-Eye Institute’s ongoing efforts to connect optometry with neuroscience.
Deborah Zelinsky, O.D.
Founder, Executive Research Director
The Mind-Eye Institute
Northbrook, Illinois
Media